The most common allegations in anesthesia claims
We reviewed more than 600 anesthesia claims that closed from 2007–2012.
The most common allegation was improper performance of anesthesia procedures (25 percent). The five most common procedures associated with this allegation were injection of anesthesia into spinal canal (37 percent), intubation of respiratory tract (35 percent), injection of anesthesia into a peripheral nerve (20 percent), injection of anesthesia into a sympathetic nerve (3 percent), and nasopharyngeal intubation (2 percent). Physician reviewers agreed that technical performance was a major factor contributing to patient harm. However, they viewed these technical issues as being mostly known complications (80 percent)—complications the patient was aware of before the procedure—and not due to negligence. Only 20 percent of the cases in this category (9 percent of all anesthesia cases) were attributed to substandard performance of an anesthesia procedure.
The second most common allegation was tooth damage related to intubation or extubation (24 percent). In these cases, patients alleged damage to teeth, crowns, implants, and bridges. Many of these cases involved difficult intubations or poor condition of the teeth, but these cases were difficult to defend if the documentation failed to reference the difficult intubation or the condition of the teeth.
The third most common allegation, improper management of the patient under anesthesia, is related to decisions made by anesthesia professionals while patients were under anesthesia (19 percent). Examples include inadequate monitoring of vital signs, delayed response to obstructed ventilation or esophageal intubation, delayed response to deteriorating vital signs, and inadequate response to hemorrhage and respiratory or cardiac arrests.
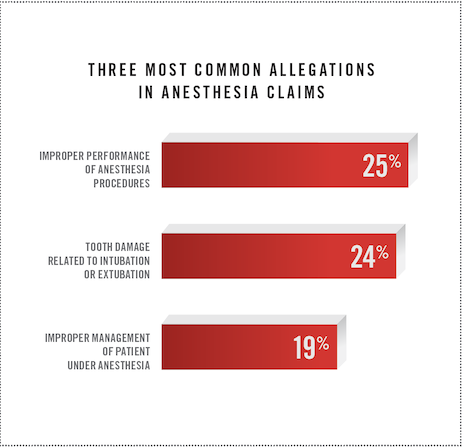
The top three allegations account for 68 percent of claims. Other allegations included failure to monitor patient’s physiological status, incorrect patient positioning, and improper choice of anesthesia.
A PDF version of this document is available here.
Detailed Discussion of Claims Findings
Although the safety of anesthesia care has significantly improved over the years, we found that patients still suffer injuries related to administration of anesthesia. The severity of injuries ranged from minor to severe—from chipped teeth to paralysis, brain damage, and death.
Technical performance (44 percent) was identified as the most frequent cause of patient injury. This statistic is misleading, however, because three-fourths of these cases involved complications that the patient knew were risks of the procedure prior to surgery. These complications were not necessarily due to negligence. However, the other 25 percent of injuries were due to poor technique, incorrect body positioning, or inappropriate method of administering a drug/anesthetic.
Inadequate patient assessment (15 percent) was the next most common factor that contributed to patient injury. This included inadequate history and physical for patients with conditions that increased the risk of complications and unanticipated outcomes. It also included failing to note available clinical information, such as abnormal EKGs, elevated potassium, and pulmonary artery stenosis, that resulted in patient injury.
The third most common problem associated with patient injury waslack of documentation (14 percent. Documentation was missing for clinical findings such as low blood pressure and oxygen saturation. Experts also noted inadequate documentation of care in situations such as resuscitation attempts.
There are several possible explanations for gaps in documentation: anesthesia professionals were not monitoring patient vital signs, were distracted, or failed to note what they were observing. Gaps in documentation imply inadequate vigilance, thus sometimes making these cases difficult to defend.
Failures in documentation may contribute to the fourth most common factor,inadequate patient monitoring (12 percent). This was seen in cases where there were drops in vital signs or end-tidal CO2 values with no response from the anesthesiologist for an unreasonable amount of time. There were also delays in response to clinical alarms, which were either disregarded, turned off, or not heard.
The fifth most common factor that contributed to patient injury waspatient factors (10 percent. Most of these factors were related to the patient anatomy, causing difficult or delayed intubations and difficulty placing regional anesthetics. Other patient factors were comorbidities, such as obesity, cardiovascular disease, diabetes, chronic pulmonary disease, smoking, hypertension, and sleep apnea.
Common themes
A common theme in this study was inadequate preparation for complications. For example, the appropriate equipment was missing when patient anatomy made it difficult to intubate and delays caused an anoxic event. In a few of these cases, rescue was delayed because equipment for emergency tracheostomies or cricothyrotomies was not readily available. Responses were delayed when blood and blood products had not been ordered for patients with clotting disorders or impaired clotting mechanisms due to medication.
Regional anesthesia has its own set of risks. Infrequent problems identified in these claims include incorrect placement of anesthetic agents, incorrect agent infusion, and incorrect doses. Patients suffered reactions to anesthetic agents, experienced nerve damage from swelling or tourni-quet pressure, and experienced bleeding or pneumothorax from punctures due to incorrect placement of needles.
Extubation resulted in harm if too much medication was given in close proximity to the time of extubation. Some of these patients suffered anoxic brain damage when they slipped into a coma due to sleep apnea, overdose of opioids, or drug reactions.
There were also problems with loss of the airway if extubations were performed too soon after surgery. Some patients had anatomic structures, such as thick necks, that had made the initial intubation difficult. Reintubation was even more challenging in a crisis or in patients who had swelling or bleeding around the airway.
Patients who had obstructive sleep apnea were at increased risk. Some patients who had been diagnosed with sleep apnea were not monitored in the hours following surgery or were discharged home. Some slipped into a coma and suffered brain damage or death. Often, these patients were given opioids for pain control, which increased risks when the patients were not monitored. Patients who had not been screened for sleep apnea and expired unexpectedly may have had undiagnosed sleep apnea. When no other cause of death was found, sleep apnea was presumed to be a likely cause.
The results of this study reveal risks to patients and exposures for anesthesiologists and CRNAs. The goal of this study is to alert anesthesia professionals to risks that can be addressed to help prevent patient harm.
By Darrell Ranum, JD, CPHRM, Vice President, Department of Patient Safety
By David B. Troxel, MD, Medical Director, Board of Governors
The guidelines suggested here are not rules, do not constitute legal advice, and do not ensure a successful outcome. The ultimate decision regarding the appropriateness of any treatment must be made by each healthcare provider in light of all circumstances prevailing in the individual situation and in accordance with the laws of the jurisdiction in which the care is rendered.